Patient Education
At Virginia Lung, our mission is to provide personalized, compassionate and comprehensive pulmonary services to our patients by focusing on prevention, diagnosis and cost effective treatment from respiratory ailments. We strive to nurture the respiratory health of our patients, neighborhood and communities, one patient at a time!
Request an AppointmentAsthma
Asthma is a chronic respiratory condition characterized by inflammation of the airways, leading to recurrent episodes of wheezing, breathlessness, chest tightness, and coughing. It is caused by a combination of genetic and environmental factors. This common condition affects people of all ages and can vary in severity, with some individuals experiencing mild, intermittent symptoms, while others may face more persistent and severe breathing problems.
The hallmark of asthma is the inflammation of the bronchial tubes, which results in the narrowing of air passages. Triggers, such as allergens, smoking, pollutants, respiratory infections, seasonal changes or physical exertion, can exacerbate symptoms by causing the muscles around the airways to tighten further and increasing mucus production. These episodes, known as asthma attacks, can range from mild to severe, requiring prompt medical intervention.
While there is no cure for asthma, various effective management strategies exist to control symptoms and improve quality of life. Long-term control medications, such as inhaled corticosteroids, leukotriene modifiers, and bronchodilators, play a crucial role in preventing inflammation and maintaining open airways. Additionally, individuals with asthma are often encouraged to identify and avoid triggers, adopt a healthy lifestyle, and have an individualized asthma action plan to respond to worsening symptoms.
Biologics are a more recent breakthrough in asthma treatment, offering targeted therapy for individuals with uncontrolled symptoms. These specialized drugs, typically administered through injections, target specific molecules involved in the inflammatory process of asthma therefore reducing airway inflammation and preventing asthma exacerbations. In the right population of patients, these drugs significantly improve the quality of life by mitigating symptoms, reducing reliance on systemic steroids, and minimizing the risk of severe attacks.
Regular medical follow-ups, patient education, and advancements in treatment options contribute to better asthma management, allowing individuals to lead active and fulfilling lives despite the challenges posed by this chronic respiratory condition.
COPD
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung condition that significantly impacts breathing. It causes your airways to become inflamed and narrowed, making it difficult to exhale fully. The two main forms of COPD are chronic bronchitis and emphysema, often coexisting in individuals.
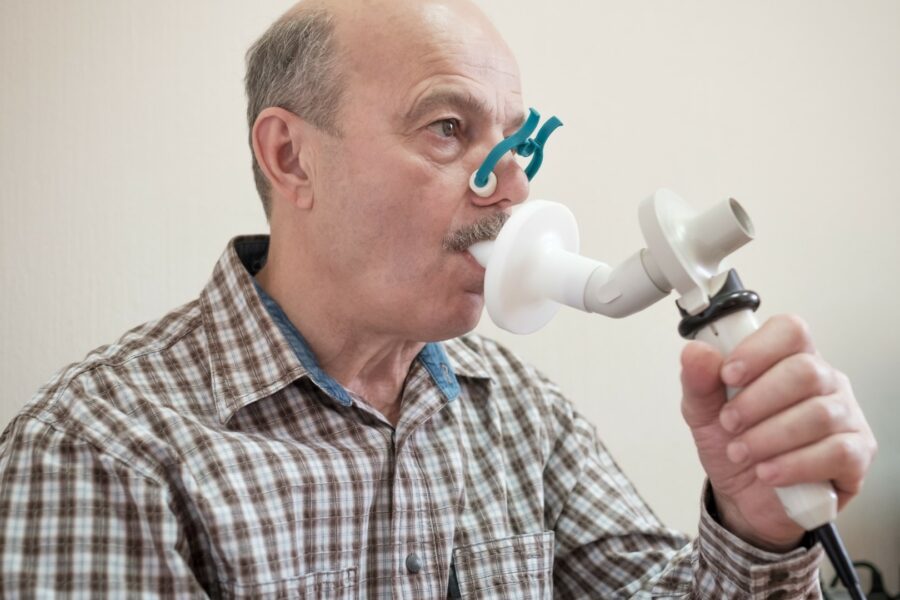
Smoking is the primary cause of COPD, but long-term exposure to lung irritants such as air pollution, chemical fumes, or dust can also contribute. Early diagnosis is crucial, typically involving pulmonary function tests and imaging studies, to assess lung function and rule out other conditions.
Common symptoms include persistent cough, excessive production of mucus, shortness of breath (especially during physical activity), wheezing, and chest tightness. These symptoms tend to worsen over time, leading to a decreased ability to perform daily activities and, in severe cases, can result in respiratory failure.
Management of COPD revolves around lifestyle changes, including smoking cessation and regular physical activity. Medications such as bronchodilators and corticosteroids are often prescribed to alleviate symptoms and reduce inflammation. In advanced cases, oxygen therapy or surgical interventions may be considered. Patient’s may also benefit from referral to Pulmonary Rehabilitation. Pulmonary rehabilitation is a comprehensive program designed to improve the well-being and functionality of individuals with chronic respiratory conditions, such as chronic obstructive pulmonary disease (COPD). This structured intervention combines exercise training, education, and behavioral strategies to enhance lung function, reduce symptoms, and enhance overall quality of life.
It’s essential to work closely with healthcare providers to develop a personalized treatment plan, attend regular check-ups, and stay vigilant about respiratory infections.
COVID-19
COVID-19, caused by the novel coronavirus SARS-CoV-2, emerged as a global pandemic, profoundly impacting societies worldwide. The virus primarily spreads through respiratory droplets, leading to a range of symptoms from mild respiratory issues to severe pneumonia, acute respiratory distress syndrome (ARDS), and in some cases, death. The virus can also affect multiple organs beyond the respiratory system.
Key symptoms include fever, cough, and shortness of breath, with variations in severity. Asymptomatic carriers can unknowingly contribute to transmission, making containment challenging.
If you suspect you have COVID-19 or are experiencing symptoms such as fever, cough, shortness of breath, or loss of taste or smell, it is essential to seek medical advice promptly. Contact your healthcare provider or local health department for guidance on testing.
Testing for COVID-19 typically involves a nasal or throat swab. Some tests provide results within minutes, while others may take a day or more.
Getting vaccinated against COVID-19 is a key preventive measure. Vaccines have proven effective in reducing severe illness, hospitalization, and death.
Outpatient treatment for COVID-19 primarily focuses on managing symptoms, preventing the spread of the virus, and addressing any underlying health concerns. It’s crucial to note that the specific treatment plan may vary based on individual circumstances and the severity of symptoms. General guidelines include:
Isolation: Stay at home and isolate yourself from others, including family members, to prevent the spread of the virus.
Hydration/Rest: Get plenty of rest to help your body recover. Stay well-hydrated by drinking fluids like water, herbal teas, and clear broths.
Over-the-counter medications: Use over-the-counter medications to alleviate symptoms. Acetaminophen or ibuprofen can help reduce fever and relieve pain. Follow your healthcare provider’s recommendations for dosage and duration.
Monitor symptoms: Keep a close eye on your symptoms, especially respiratory symptoms like shortness of breath. If able, use a pulse oximeter to monitor your oxygen saturation levels at home, if advised by your healthcare provider.
Telehealth monitoring: Participate in telehealth appointments with your healthcare provider for regular check-ins and to discuss your symptoms. Report any concerning symptoms promptly.
Antiviral medications: In some cases, healthcare providers may prescribe antiviral medications, such as remdesivir, for certain high-risk individuals or those with severe illness. The decision to use these medications is individualized and based on various factors.
Follow-up: Attend any follow-up appointments scheduled by your healthcare provider. Communicate any changes in symptoms or concerns during follow-up appointments.
Emergency care: Seek emergency medical attention if you experience severe symptoms, such as difficulty breathing, persistent chest pain or pressure, confusion, inability to stay awake, or bluish lips or face.
Interstitial Lung Disease
Interstitial lung disease (ILD) is a group of disorders affecting the tissue and space around the air sacs (alveoli) in the lungs. These disorders lead to inflammation and scarring (fibrosis) in the lungs, hindering their ability to expand and contract efficiently.
Common symptoms include persistent dry cough, shortness of breath (especially during activity), fatigue, and chest discomfort. Diagnosis of ILD involves a thorough examination, pulmonary function tests, imaging studies, blood tests and sometimes a lung biopsy to identify the specific type of interstitial lung disease.
While the causes of ILD can vary, exposure to environmental factors like asbestos, certain medications, autoimmune diseases, and genetic factors may contribute. Management often involves addressing the underlying cause, if possible, and utilizing medications such as corticosteroids or immunosuppressants to reduce inflammation and slow the progression of fibrosis. Sometimes anti fibrotic agents are also used to slow down progression.
Pulmonary rehabilitation programs, supplemental oxygen therapy, and lung transplant may be considered for advanced cases. Regular follow-ups with healthcare providers are crucial to monitor symptoms, adjust treatment plans, and enhance overall well-being.
Patients with ILD are encouraged to adopt a healthy lifestyle, including smoking cessation and staying physically active as much as possible. Collaborating closely with your pulmonologist and staying informed about ILD can empower individuals to manage their condition effectively and maintain an optimal quality of life.
Lung nodules and lung cancer
Pulmonary nodules are small growths in the lungs that are often incidentally discovered during imaging studies, such as chest X-rays or CT scans. While most nodules are benign, some may be early signs of lung cancer. The risk of a pulmonary nodule being due to cancer is determined by factors like nodule size, appearance, and the patient’s medical history.
The evaluation of pulmonary nodules involves a thorough assessment, including imaging studies, such as CT scans, and sometimes additional tests like positron emission tomography (PET) scans or biopsies to determine their nature. Notably, the management of pulmonary nodules and lung cancer varies based on factors such as size, growth rate, and the likelihood of malignancy.
Lung cancer is a complex and potentially lethal condition characterized by the uncontrolled growth of cells in the lungs. It is often associated with tobacco smoking, but non-smokers can also develop lung cancer. Symptoms may include persistent cough, chest pain, shortness of breath, and coughing up blood. Early-stage lung cancer is frequently asymptomatic, underscoring the significance of routine screenings for high-risk individuals.
Treatment for lung cancer may involve surgery, chemotherapy, radiation therapy, or a combination, depending on the cancer’s type and stage. Collaborating closely with healthcare providers for personalized assessments and timely intervention is crucial for effectively managing pulmonary nodules and improving outcomes in lung cancer cases.
Pleural effusion
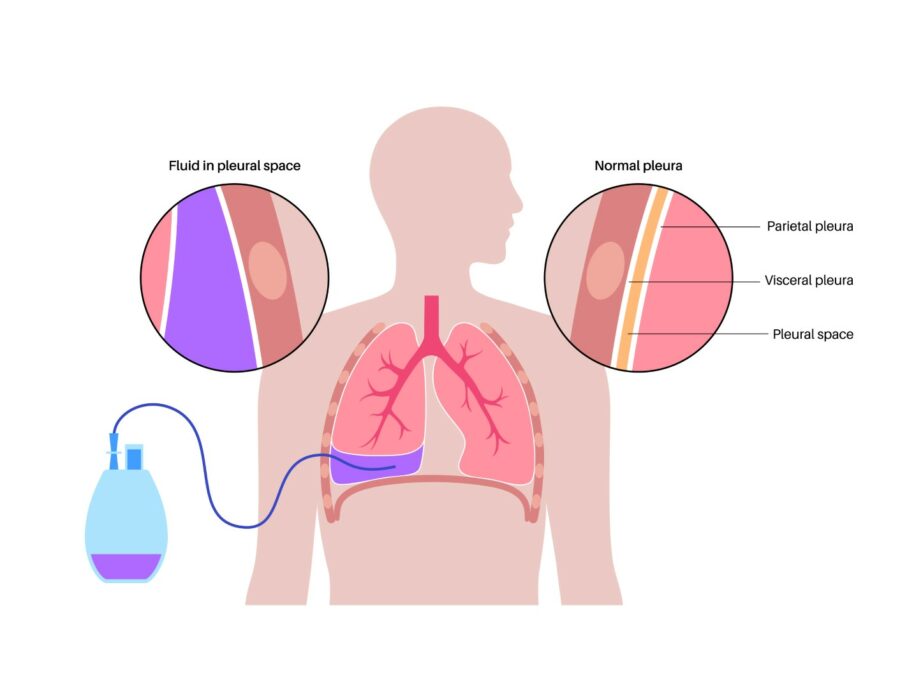
Pleural effusion refers to the abnormal accumulation of fluid in the pleural space, a thin membrane surrounding the lungs. This condition arises from various underlying causes, including infections, heart failure, kidney disease, malignancies, and inflammatory diseases. As the fluid accumulates, it compresses the lungs, leading to breathing difficulties and chest discomfort.
Common symptoms include shortness of breath, chest pain, and cough. Diagnosis involves physical examination, imaging studies like chest X-rays or CT scans, and sometimes thoracentesis, a procedure to drain and analyze the fluid.
Thoracentesis is a medical procedure in which a thin, hollow needle or catheter is inserted through the chest wall into the pleural space to remove excess fluid. During thoracentesis, the patient typically sits upright or leans on a bedside table while a healthcare provider numbs the skin on the back or side of the chest. Using imaging guidance, such as ultrasound, the healthcare provider carefully inserts the needle or catheter into the pleural space to drain the fluid. The collected fluid is then sent to a laboratory for analysis to determine the underlying cause of the pleural effusion.
Treatment depends on addressing the underlying cause; it may involve medications, drainage procedures, or surgical intervention.
Pneumonia
Pneumonia is a respiratory infection characterized by inflammation of the air sacs in one or both lungs, typically caused by bacteria, viruses, and rarely fungi. The condition interferes with the normal functioning of the lungs, leading to the accumulation of pus in the air sacks, leading to shortness of breath. Common symptoms include cough, chest pain, fever, and difficulty breathing. Pneumonia can affect individuals of all ages but poses a greater risk to the elderly, young children, and those with weakened immune systems. Diagnosis involves clinical evaluation, chest X-rays, and sometimes blood tests or sputum cultures to identify the causative agent.
Treatment varies based on the type of pneumonia and its underlying cause. Bacterial pneumonia is often treated with antibiotics, while antiviral medications are employed for viral pneumonia. Supportive measures such as rest, hydration, and pain management play a crucial role in recovery. Severe cases may require hospitalization, particularly for individuals with compromised immune systems or pre-existing health conditions. Vaccination against common pathogens, such as Streptococcus pneumoniae and influenza viruses, is a key preventive measure.
Prompt medical attention is essential to prevent complications and ensure a timely recovery.
Pulmonary hypertension
Pulmonary hypertension (PH) is a complex and progressive condition characterized by elevated blood pressure in the pulmonary arteries that supply blood to the lungs. Normally, these arteries carry oxygen-depleted blood from the heart to the lungs for oxygenation. In pulmonary hypertension, however, the walls of the pulmonary arteries thicken and narrow, leading to increased resistance to blood flow.
There are various causes of pulmonary hypertension, broadly classified into five groups. Group 1, or pulmonary arterial hypertension (PAH), involves abnormalities in the small arteries of the lungs, often with no apparent underlying cause. Other groups include PH associated with heart diseases, lung diseases, chronic blood clots, or other systemic disorders. The increased pressure in the pulmonary arteries puts strain on the right side of the heart, leading to right heart failure if left untreated.
Common symptoms of pulmonary hypertension include shortness of breath, fatigue, dizziness, and chest pain. Diagnosis typically involves a combination of medical history, physical examination, imaging studies, and specialized tests such as right heart catheterization.
While there is no cure for pulmonary hypertension, treatment aims to alleviate symptoms, improve quality of life, and slow down disease progression. Medications, lifestyle modifications, and in some cases, surgical interventions may be part of the management plan. Regular monitoring and early intervention are crucial in effectively managing pulmonary hypertension and preventing further complications.
Sleep medicine and OSA
Sleep medicine is a specialized field dedicated to the diagnosis and treatment of sleep disorders, which can significantly impact an individual’s overall health. Sleep disorders encompass a broad range of conditions, including insomnia, sleep apnea, narcolepsy, restless legs syndrome, and parasomnias.
Patients seeking help for sleep-related issues often undergo a thorough evaluation, which may include sleep studies conducted in a sleep laboratory or home setting. One common disorder addressed by sleep medicine is obstructive sleep apnea (OSA). OSA is a sleep disorder characterized by repeated interruptions in breathing during sleep. It occurs when the muscles in the throat relax excessively, causing a temporary blockage of the airway. Common symptoms include loud snoring, abrupt awakenings accompanied by choking or gasping, and excessive daytime sleepiness
A home sleep study is a portable and convenient diagnostic tool for assessing sleep disorders. It involves using a compact device that measures key indicators such as breathing patterns, oxygen levels, heart rate, and body movement while the individual sleeps in their own bed. This unobtrusive method offers a more natural sleep environment, increasing the likelihood of capturing accurate data. While it may not be as comprehensive as an in-lab polysomnography, a home sleep study is a valuable and cost-effective alternative for diagnosing conditions like sleep apnea, allowing individuals to undergo testing in the comfort of their homes.
Treatment approaches vary depending on the specific sleep disorder diagnosed. For instance, continuous positive airway pressure (CPAP) therapy is a common intervention for OSA.
Consulting a sleep medicine doctor can provide individuals with personalized strategies to optimize their sleep and enhance their overall quality of life.